By Patrick Krause
“How can we use behavioral insights to nudge individuals into better health decision making?”
This is one of the fundamental questions that inspired the third annual Conference on Behavioral Economics (BE) in Global Health at UC Berkeley, organized by the Behavioral Economics in Reproductive Health Initiative (BERI) at the Center for Effective Global Action (CEGA).The wide range of presentations included the use of monitoring and incentives to increase hand washing in West Bengal, masculinity priming in advertising & cash incentives to increase take up of voluntary medical male circumcision in South Africa, and the potential negative spillovers of incentivizing healthy food choices for American primary school children (follow link to event page to find all event materials and videos of the presentations, also here.) Here are some key takeaways from the conference:
As many of you reading this may know, BE has made its way into the realm of global health at many large US-based institutions, making it an exciting time at for us at BERI. The conference included presenters from the World Bank’s Global INsights Initiative (GINI), and The White House Social & Behavioral Science Team (aka “the nudge unit”). Kama Garrison (USAID) presented on the ongoing collaborations between the White House nudge unit and USAID, and how they are using BE to inform and strengthen traditional health focused Social & Behavioral Change Communication (SBCC) interventions. The majority of rigorous impact evaluations undertaken by these new groups are still ongoing in the field and have not yet generated evidence, but the increased incorporation of BE into solving health and gender related issues makes it a very exciting time.
A major theme of many presentations was evaluating methods to combat individuals’ inconsistencies in valuation of present cost vs. future benefits (i.e. “present bias”, see BERI conceptual framework for how to think about this in the context of Family Planning and Reproductive Health). We, as humans, tend to place greater value on the costs/benefits to present actions, and tend to have a very hard time properly discounting the same costs/benefits of future actions. Thus we severely underestimate future costs, relative to present costs, especially when the future costs are uncertain.
Present bias can explain individuals procrastinating investing in preventative healthcare (even though they know it will make us healthier in the long-run), why it is hard to quit smoking (aside from the physical addiction), or why some women may not utilize family planning services or modern contraceptives (even when they do not want to get pregnant). As you can see, these decisions influenced by present bias can have serious negative impacts on health outcomes for individuals and communities. In some ways I think of addressing this present bias as low-hanging fruit for improving a number of current health interventions. If this bias is could be addressed, it could would result in a large increase in take up of the intended health input with, in some cases, only minor tweaks to existing programs.
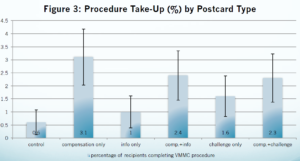
VMMC procedure take-up by treatment arm
At the conference, we learned that small monetary incentives can be a powerful tool in addressing present bias and encouraging positive behaviors. In Nick Wilson’s presentation we saw that small monetary incentives had a large positive effect on the take up of Voluntary Medical Male Circumcision (VMMC) in high-risk HIV populations in South Africa. VMMC can be a powerful tool in fighting HIV, as it can lower transmission by 51-76%.While the World Health Organization (WHO) is trying to scale up VMMC interventions (free provision) in 14 priority countries, current take up of the procedure is extremely low. When males were offered a conditional $10 (100R) incentive to attend a VMMC counseling session, it tripled the take up of the counseling session. Further, approximately 90% of those that attended the informational sessions went on to have the procedure. This result implies there was pent-up demand for the procedure, that was being held back by procrastination, most likely caused by present bias. The conditional monetary incentive transferred a very tangible benefit of VMMC to the present, which was enough to overcome the temporal mismatch of costs / benefits due to present bias.
Small incentives also were shown to help combat behavioral biases in other studies as well. A form of a small incentive, lottery tickets, was shown to have a large increase in hand washing practices in West Bengal as well. Prior to the intervention, the majority of individuals surveyed rinsed their hands with water. However, very few took the extra step of using soap, despite understanding the added health benefits. Therefore, the lack of hand washing was not due to lack of information, but was most likely driven by behavioral biases.
Although there were many positive examples that showed small incentives were beneficial in nudging individuals’ choices, other examples proved them inefficient, dispelling the myth that they were a “silver bullet” to nudge individuals into acting in a way that would lead to better health outcomes.
Julian Jamison’s presentation showed us that the same exact intervention can have drastically different outcomes in different contexts, even within the same country. The intervention tested the effectiveness different behavioral incentives (social recognition vs. lotteries) to increase record keeping performance of public health clinic works in two Nigerian states (Ekiti & Niger). The socio-economic and geographical make up of these two states are quite different from each other. His results show that while the social recognition intervention had a positive impact on performance in Ekriti, there was no impact on performance in Niger.
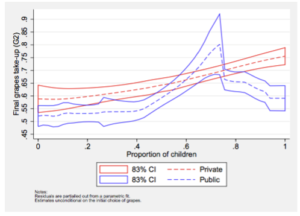
Proportion of children that selected grapes over cookies based on the proportion of children that received the incentive
Anya Samek’s presentation exhibited that when incentives are made public knowledge and available to everyone, there is a potential for negative spillovers. Her results showed that when public incentives for healthy food choices (such as giving a child a toy for choosing grapes over cookies) were made available to all children, there was lower take up of the healthy food choice than when the incentive was only offered to half of the children. Yet, we don’t see this outcome when the incentives remained private. These results illustrate that incentives may serve as a signal that the incentivized choice (the healthier option) is inferior or undesirable. Or, it could mean that the present benefit of the toy was valued less by the kids when everyone was able to get it (making it no longer special), so the immediate benefit of a sugar rush from the cookie won out.
Incentives can also have an impact on the price or value that individuals place on a product or service. In the previously discussed hand washing study, the participants that received incentives were less willing to pay for hand soap at the end of the study, than those who did not receive incentives.
In one of my favorite results presented at the conference, one arm of the previously discussed VMMC intervention used advertisements that framed the take up of the counseling as a challenge to the man’s masculinity. To do this, the researchers included the phrase “Are you tough enough?” on a flyer promoting circumcision. This “masculinity framing” roughly doubled the take-up of the consultations/procedure (compared to the control group), slightly less than the monetary incentive arm (tripled take-up). This shows that the both the framing of advertisements and providing monetary incentives can be powerful tools in addressing present bias and increase preventative health action.
 vs
vs 
Can you guess which one was more effective for increasing procedure take up?(source)
Finally, we saw the act of monitoring behavior and/or providing feedback had effects on behaviors in some studies. Simply telling people that they were going to be monitoring people increased the rates of hand washing, compared to the control group (who didn’t know they were being monitored). Further, providing feedback on performance (for those in the control group) improved record keeping performance of the clinic works, though the improvement was statistically less than the social recognition treatment group. These are interesting result that make me think about the Hawthorne effect for these types of Randomized Control Trials (RCTs) in general.
Overall the conference showed the potential for applying behavioral insights to many of the global health challenges we currently face, and we are excited that more people/intuitions are utilizing them.


